Note: Supplemental materials are not guaranteed with Rental or Used book purchases.
Purchase Benefits
What is included with this book?
The New copy of this book will include any supplemental materials advertised. Please check the title of the book to determine if it should include any access cards, study guides, lab manuals, CDs, etc.
The Used, Rental and eBook copies of this book are not guaranteed to include any supplemental materials. Typically, only the book itself is included. This is true even if the title states it includes any access cards, study guides, lab manuals, CDs, etc.
Thirteen
SARS
March-July 2003, Hanoi and Bangkok
Joel Montgomery pulled the trays that had been set aside for him out of the lab refrigerator, and winced. The trays were full of plastic bags. The bags were full of tubes of blood, labeled with the names of patients and the dates the blood had been drawn from their veins. Some of the tubes had popped open, and the blood inside them had pooled and clotted in the bottom of the bags. The labels had soaked up the blood, and some of them had slipped free of the tubes they were meant to identify. There were almost thirty bags, and more than eight hundred tubes of blood.
The tubes were resting inside a refrigerator in a high-ceilinged, marble-floored laboratory at the National Institute of Hygiene and Epidemiology in Hanoi. They represented a day-by-day record of what had gone on inside the bodies of the first group of people recognized as victims of severe acute respiratory syndrome. The blood in the tubes contained valuable information that could help the CDC understand how the virus that caused SARS evaded the immune system, and how the disease progressed.
The EIS had shipped Joel to Hanoi to help get that information. The blood had to be extracted from the tubes, spun down for its serum, divided into fractions, and shipped off to laboratories that had the facilities to analyze it safely and fast. The need for data was urgent. It was late March. The disease had been leaping around the globe for more than a month, but it had been detected and named only two weeks earlier, and the virus that caused it had been identified only four days ago. Worldwide, more than 1,300 people were known to be ill. Here in Vietnam, three nurses and a doctor were dead, fifty-five of their colleagues and relatives were hospitalized, and the hospital where they had all worked had locked its doors with its sick staff still inside. It was the hospital staff's blood that lay in the refrigerated tubes.
There was no way of knowing at this point how much virus the blood contained, or how hazardous exposure to it might be. Joel slid a Tyvek hood over his head and settled the seal of its faceplate around the bones of his jaw and cheeks. He switched on the motor of the air supply, took a deep breath, and got to work.
-- -- --
Johnny Chen was very sick, and none of the health workers treating him were quite sure why.
It was the morning of March 3, a Monday. It was early, but Hanoi is a town that rises early. The neighborhood loudspeakers that play inspirational music and scold residents for littering had crackled to life before 6:00 a.m. Dr. Vu Hoang Thu, a forty-three-year-old internist, had downed a small cup of dark filtered coffee and left the house she shared with her husband and two teenage sons before the sun pierced between the tree trunks in Lenin Park in the center of town. She was at the French Hospital, a rounded, blocky building of pink and white stucco that lay across a wide boulevard from the park, before the nurses on the night shift handed off the care of their patients to the staff coming in for the day.
Vu was one of the physicians assigned to the fifty-six-bed hospital's general medical ward. Chen was one of her patients. The forty-seven year-old American had been at the hospital for almost a week. He had checked himself in the previous Wednesday, choosing the small private institution over the sprawling, scruffy campus of state-run Bach Mai Hospital next door. He was a businessman, based in China, so he could afford the French Hospital. He had started to feel sick, with a high fever and a puzzling fatigue, immediately after arriving from Hong Kong two days before.
Slowly but steadily, Chen had gotten worse. Despite antipyretics, his fever had stayed stubbornly high. Despite antibiotics, his lungs were slowly filling with fluid; on X-rays, Vu could see the opaque shadow of inflammation moving slowly up his chest. A blood test suggested he might be infected with influenza B, the influenza virus variety that was most common in Asia; influenza B was a milder variety than influenza A, which caused wide-ranging epidemics in the Northern Hemisphere most winters. Based on the influenza test result, the staff had given him an antiviral drug, but there was no sign it had helped. On Saturday he started to cough explosively. On Sunday morning, he slipped into severe respiratory distress. He was lethargic and having trouble breathing. His skin had a greyish tinge, and when he tried to speak, he made no sense.
Clearly he was not getting enough oxygen. Vu ordered Chen put on a ventilator. It was a quick process when it went smoothly, but it was always tense. It was easy to make a mistake, and a doctor had to go nose-to-nose with the patient to sight clearly down the airway. This intubation had gone well. One nurse sedated Chen and gave him an injection that briefly paralyzed him. Another stood by his shoulder, pressing down on his throat cartilage to close his esophagus so the tube would not go the wrong way. A doctor slid the curved laryngoscope into his mouth, squinting down its sights and easing the tube along its guiding stylet, down his throat and between his vocal cords. Within moments, Chen was hooked to the ventilator. Almost immediately, his color began to improve.
That had been the day before. So when she reached the hospital, Vu was surprised to find that Chen was no better: The machine was suplying him with oxygen, but he was still obviously severely ill. There was another surprise awaiting her. One of the nurses who had assisted with his intubation was tired and had a high fever, and she was beginning to cough.
-- -- --
All over Asia that month, doctors were concerned about influenza.
One week before Chen checked into the French Hospital, the government of Hong Kong announced that two members of a local family were infected with a strain of influenza known as H5N1. The father of the family, thirty-three-year-old Ko Yan-Kit, had died in Hong Kong's Princess Margaret Hospital on February 16. Ko's wife, ten-year-old daughter, nine-year-old son, and father were also ill. Their youngest child, eight-year-old Mei-ling, was dead; she had died of pneumonia February 4, during a family visit to a small town in Fujian province north of Hong Kong.
There were two worrisome pieces of news in the family's misfortune. The first was the presence of H5N1. It was a strain of influenza A, the most common of the three types of flu virus, but it was not a strain that was supposed to show up in people. In the decades since 1933, when the flu virus was identified, research had shown that there were fifteen subtypes of influenza A, but that humans caught only three of them: H1, H2, and H3. (The H stood for hemagglutinin, a protein on the surface of the virus; the N that followed after it stood for neuraminidase, a second surface protein.)
H5N1, the strain found in the Ko family, was a disease of chickens. It was an ugly disease. It was also called "highly pathogenic avian influenza," and it deserved the name: It was fast-moving and fatal and could destroy a flock in days. An influenza expert had once described it as "chicken Ebola." H5N1 was not supposed to infect people, but it had at least once before. In the fall of 1997, it jumped species, infecting eighteen people in Hong Kong and killing six of them before the local government slaughtered every chicken in the territory and shut the outbreak down.
The episode had shaken world health authorities, and not just because it had killed one out of every three victims. Flu experts lived in terror of a new strain of the virus, one that would sweep the world in a global pandemic. The "Spanish" flu of 1918 had done that, and left 40 million dead in its wake. And a strain that jumped from another species was as novel as could be imagined. Human immune systems would have no protection against it, and existing vaccines would have no power to stop it.
The second piece of bad news was the probable location of the Ko family's infection. They were likely, based on the usual incubation period of flu, to have acquired the disease while visiting relatives in Fujian. It was a setting to make a flu scientist shudder. Outside its main city, Xiamen, much of Fujian is rural and agricultural, full of small villages where residents keep a pig and a few chickens or perhaps some ducks. By a quirk of biology, pigs are vulnerable not only to the influenza viruses specific to swine, but to human and bird flu viruses as well. If a pig is infected by several subtypes of influenza at once, the viruses can swap genes, potentially producing a novel flu strain that carries the lethality of avian influenza and the contagiousness of human flu.
Over the years, researchers had noted that most of the world's new flu strains originated in southern China, and they feared the potential of China's backyard agriculture to brew even more new viruses. If the Ko family had been infected in Fujian and had brought the virus back to Hong Kong, the implications were grave indeed.
-- -- --
The concerns about influenza were not limited to Hong Kong.
The previous November, a puzzling respiratory illness had started cropping up in Guangdong, the province south of Fujian. Guangdong wraps around Hong Kong on three sides, and its border with the territory is porous because the province, and especially its capital Guangzhou, is the fervent center of China's new capitalism. Guangzhou holds more than 5 million people. Its downtown is a maze of skyscraper construction, even though the near outskirts are as humble as the villages in Fujian.
The cases of illness started in Foshan, a fast-growing town of more than 3 million that lies southwest of Guangzhou. Week by week, the unexplained pneumonia spread through the countryside of the Pearl River Delta. The stories that appeared in the state-run newspapers -- in Zhongshan, south of Guangzhou, and Heyuan, north of the city -- denied the outbreak's existence so vociferously that they effectively confirmed its existence. Rumors that health care workers were sick became so common that the World Health Organization asked the Chinese Ministry of Health to comment. The reply that came back by email said there was only a minor outbreak of influenza B.
On February 3, a forty-year-old man checked himself into the No. 2 Hospital in Guangzhou. His lungs were filling up from pneumonia and he was coughing and feverish. The illness spread rapidly through the hospital. Within two weeks, there were enough health care workers sick with the same unexplained ailment to fill an entire ward. The remaining staff were frantic. They worked long hours, trading back and forth between their sick colleagues and the steady flow of patients coming in from outside.
By the second week of February, the rumor of the outbreak had reached a new audience: the Internet. In a chat room on a site called Teachers.net, a California fourth-grade teacher named Catherine Strommen received a note from a Guangzhou teacher she had spoken with a few times before. The note asked: "Have you heard of the terrible sickness in my city?"
She had not, but she thought she knew someone who might. Strommen's husband had been in the Navy, and they had once been assigned to Hawaii where they made friends with a Navy physician and epidemiologist who lived nearby. The neighbor, Dr. Stephen O. Cunnion, was now an international health consultant in suburban Washington. He relayed her question to ProMED, a listserv for reporting disease outbreaks that is run by the International Society for Infectious Diseases and has more than thirty thousand subscribers worldwide.
After vetting by the moderators, Cunnion's post appeared the next day, February 10. It quoted Strommen's note: " 'Have you heard of an epidemic in Guangzhou? An acquaintance of mine...lives there and reports that the hospitals there have been closed and people are dying."'
Cunnion got dozens of replies, though none from China. But less than a day later, the Guangdong Department of Health made its first official statement about the outbreak.
Yes, the agency said, there had been an outbreak of about three hundred cases of pneumonia and five deaths, but it was ending. In fact, it was not ending, though no one outside China would learn that for six more weeks. It had spread to at least eight cities within Guangdong. At the No. 2 Hospital, more than fifty health care workers were sick, and their healthy colleagues were growing exhausted caring for them. One of the healthy ones was Dr. Liu Jian-Lun, a sixty-four-year-old professor of medicine at Zhongshan University in Guangzhou. In late February, he took a break from the epidemic. His nephew was getting married in Hong Kong, and Dr. Liu wanted to be there -- even though, in the past few days, he had been starting to feel a little unwell.
On February 21, Dr. Liu and his wife checked into the Metropole Hotel in Kowloon, on the mainland side of Hong Kong. They were given room 911. On the ninth floor with them were a random group of travelers whose names, or fates at least, would soon become known worldwide. One of them was Johnny Chen.
-- -- --
The French Hospital, where Chen arrived five days after spending the night on the same hotel floor as Liu -- whether they ever met, or even passed in the hall, has never been established -- had become the site of a ferocious outbreak. By March 5, three days after Chen's intubation, the nurse who had helped grew so sick that she was hospitalized. By March 6, nine more of the staff had the same symptoms that she did: sudden high fever, deep malaise, nonproductive cough.
"From the fifth, we did blood tests every day, for the entire staff," Vu said. "We didn't find anything."
The medical staff had heard of the influenza cases in Hong Kong and the pneumonia epidemic on the mainland. They knew Chen had passed through Hong Kong, and they suspected he had acquired his illness there. The hospital's management called the local WHO office to let them know that something inexplicable might have crossed the border. WHO has only a small group in Hanoi, headed by an elegant Frenchwoman named Pascale Brudon. She asked a member of her staff, Dr. Carlo Urbani, to take a look.
Urbani was forty-six, a big, cheerful man with dark hair and a wide forehead who came from Castelplanio, a small town on Italy's Adriatic coast. He had spent much of his medical life in Africa and Asia, and he had come to Vietnam with his wife and three children to work on programs preventing parasitic diseases in children. He was the former president of the Italian branch of Médecins Sans fronti`eres, known in the United States as Doctors Without Borders, and had helped accept the Nobel Peace Prize given to the group in 1999. "Health and dignity are indissociable in human beings," he said at the ceremony. "It is a duty to stay close to victims and guarantee their rights."
Urbani made his first visit to the French Hospital on February 28, two days after Chen was admitted. Like the hospital staff, he had heard the news from Hong Kong, and he worried that Chen might have carried avian influenza into Vietnam. He was especially struck that health care workers were falling ill so quickly. On March 5, he sent a warning email to the WHO's communicable diseases division in Geneva, and he began coming to the French Hospital every day, sometimes twice a day. He began to worry the disease was not influenza. He kept checking the sick staff, swabbing their throats for analysis and drawing their blood, looking for a clue that would explain what was making them so ill.
Chen's family had him medevaced to Hong Kong on March 6. His departure came too late for the French Hospital. On the 7th, two more cases developed, making twelve in all, and Urbani recommended the hospital isolate its sick staff in one ward on its second floor. On the 8th, five of the twelve developed bilateral pneumonia. Urbani herded the remaining staff into the cafeteria and urged them all to wear whatever protective gear the hospital had in stock, especially face masks, at all times. On the 9th, there were fifteen cases. In a desperate bid to halt the disease's advance, the hospital turned off its air-conditioning.
On March 11, several things happened at once. The count of sick doctors and nurses rose to thirty-five; four of their family members were ill as well. The hospital did not have enough staff left to operate -- it barely had enough to care for its own sick personnel -- and so it closed its doors. Its patients were transferred to Bach Mai Hospital next door. The sick staff, most of them now gasping with pneumonia or sedated and on ventilators, stayed behind. They were accidental victims of a still-unidentified plague, and their workplace had become a plague hospital.
Inexplicably, Vu was not sick. When the hospital sealed its doors, she remained inside. She would not come out for more than three weeks.
"I stayed for my colleagues," she said. "I said to the others who were not sick that we should try to continue. But we were very worried, very scared."
On the same day, Urbani made a morning visit to the hospital, to check on the sick staff and take another set of samples. Then he hurried back to the WHO office. He was due in Bangkok that evening; he was giving a talk at a scientific meeting, a long-standing commitment, the next day.
From the airport, he called Brudon.
"He said he was not feeling very well," she said. "He said, Pascale, I think I have got this disease."
-- -- --
Urbani's first alarmed communiqué to the WHO about Chen had been shared with the CDC. So had subsequent accounts that he sent over the ensuing ten days, describing the clinical features of the health care workers' cases and the epidemiology he had pieced together of how they became infected.
He had reported Chen's illness, at first, as a suspected case of influenza -- either the avian influenza that had appeared in Hong Kong, or the influenza B that Vietnam had found in its earliest tests on Chen. The reports came into a flu office that was already on guard against the bird flu. Dr. Keiji Fukuda, the CDC's chief of influenza epidemiology and its in-house expert on avian influenza, was in Beijing at the Chinese government's invitation, ready to search for any links between the new H5N1 cases and the Guangdong epidemic. The invitation had reportedly been issued only after HHS Secretary Tommy Thompson applied polite pressure to his Chinese counterpart, the minister of health. There was certainly no evidence of an enthusiastic welcome within China: Fukuda and his WHO colleagues had been in Beijing for two weeks, but had not yet received permission from the Guangdong health department to travel there.
Urbani's notes were being read as well by Tim Uyeki, who had joined the flu branch as an EIS officer in 1998 and stayed to be a staff epidemiologist when his two years were up. Uyeki was a pediatrician, trained in Cleveland and California, who had a public policy degree as well as the standard M.D./M.P.H. combination shared by most of the CDC's physicians.
"Between the incubation period and some of the other clinical features Urbani described, we didn't think it sounded like influenza," Uyeki said. "Especially if it was influenza B, because B doesn't cause severe outbreaks. If it was influenza B, it would have been the most severe influenza B virus in world history."
The puzzle of which pathogen lay at the heart of the outbreak increased the CDC's desire to get to Vietnam to help. But there was a hurdle in the way: It had to be asked. The investigation belonged to the WHO, and the decision to allow the WHO to bring in extra investigators rested with the Vietnamese Ministry of Health. The WHO's relationship to countries is like the CDC's to the states. It has abundant influence but little overt power; it can persuade, but not compel. On March 9, the ministry's permission arrived: It would allow the WHO to bring in two more investigators. The WHO elected to send Dr. Hitoshi Oshitani, the communicable diseases expert in its Western Pacific office, based in Manila. The CDC sent Tim Uyeki.
There was no time to get a visa. Uyeki left immediately, carting three trunks of medical supplies as well as his own bags. He headed for Bangkok, because he could enter Thailand without advance permission and because the staff there, the largest CDC group in Asia, needed to be warned of what was going on. Bangkok is a tourism crossroads, but it is also a medical hub for most of Southeast Asia. In Atlanta, the CDC's planners could envision a scenario in which a member of Asia's new super-rich was attacked by the mystery pneumonia and fled to Bangkok for care, spreading the disease to yet another country. And if the situation in Vietnam got worse, the CDC workers in Bangkok might be recruited to help.
It was very early March 11 by the time Uyeki reached Bangkok. He fought his way through the city's gridlock to Scott Dowell's office in Nonthaburi, a suburb embedded in the city's northward sprawl. In a tense meeting, Uyeki described the explosive outbreak in the French Hospital, and the little the CDC knew so far about the epidemic in Guangdong. It was eight years since the Rwandan refugee crisis, and Dowell was now chief of the Bangkok office of the International Emerging Infections Program, a group that the CDC was gradually deploying around the world as an early-warning system for unusual diseases. He had set up the office, the first one in the program, in fall 2001. After eighteen months in Thailand, he had a vivid appreciation of how quickly a new organism could take root there.
Dowell thought the Hanoi WHO representative, Bjorn Melgaard, needed to hear Uyeki's report as well. But time was short: Uyeki was leaving on an evening flight, and he still needed a Vietnamese visa and several more boxes of supplies. Melgaard squeezed them into his schedule over lunch, and listened somberly as Uyeki described CDC's concerns about the Vietnamese and Chinese outbreaks. They discussed, briefly and apprehensively, the strategies they would have to deploy if a case of the disease landed in Bangkok. Then Dowell rushed Uyeki off again.
Uyeki landed in Bangkok at about 8:00 p.m. and argued his trunks of supplies through customs. That took more than an hour. He found a taxi to take him the thirty-minute ride into the city, and went straight to the WHO office, a cream-colored modernized villa on a busy street not far from the architectural wedding cake of Hanoi's Opera House. He had expected to meet Urbani there, but the villa was dark, and the gates were locked. He had no way of knowing that he and Urbani had passed, literally, in mid-air.
At about the same time, in Bangkok, Melgaard called Dowell at home.
"What we discussed this afternoon has happened," he said. "And it is worse than you imagined. It is one of our staff."
The next morning, for the first time in ten years, the WHO issued a global alert.
-- -- --
It came too late. While the CDC and the WHO had been focused on Hanoi, the still-unexplained disease had seeded itself around the world.
On the afternoon that Dr. Liu checked into the Metropole Hotel, a Chinese-Canadian family were checking out. They lived outside Toronto, but they had been visiting their son in Hong Kong for the celebration of the Lunar New Year. They arrived home February 23. A few days later, Kwan Sui Chu, the seventy-eight-year-old mother of the family, began to feel feverish. On March 5, she died at home of a heart attack. Two days later, her son Tse Chi Kwai, felt feverish too. He sought help in the crowded emergency department of Scarborough Grace Hospital in a Toronto suburb.
Tse died March 13. His visit to the hospital started a chain of infection that would produce 251 cases of illness in Canada, and forty-three deaths.
Staying on the same floor as Dr. Liu were three young women from Singapore who had come to Hong Kong on a shopping trip. When they returned home, they sparked an outbreak that sickened thirty-four others. A Singaporean doctor who treated some of the first patients infected by the women visited New York City for a medical meeting, and then flew home through Europe. He was taken off the plane in Frankfurt, along with his pregnant wife and mother-in-law, and hospitalized there, becoming Europe's first cases of the new disease.
On the night that Dr. Liu stayed in the hotel, he attended his nephew's wedding banquet. He infected one of the other relatives there, as well as a local resident who was visiting the hotel. Both men were treated at separate Hong Kong hospitals. A visitor to one of the hospitals later took a plane to Beijing, carrying the infection into China's interior and passing it to travelers who brought it to Inner Mongolia and Taiwan.
Dr. Liu checked himself into a Hong Kong hospital on February 22. He warned the staff to put him in isolation, and he told some of them about the epidemic he had helped to treat in Guangdong. He died March 4. Thanks to Liu's visit, and an unknown number of other patients who may have crossed the border, there would eventually be 1,755 cases of the disease and 299 deaths in Hong Kong.
One of those was Johnny Chen. He died in a Hong Kong hospital on March 13, one week after being medevac'd from Hanoi.
It would take weeks for those connections to emerge. Meanwhile, in Hanoi, one of the nurses who had treated Chen died March 15. The doctor who intubated him died March 19. Fifty-six health care workers and their families were sick, at the French Hospital and at Bach Mai. The CDC and WHO were just beginning to understand the scope of what they faced.
"What was going on in that hospital was the same thing that was going on in Guangdong province, though we had no idea what it was," Uyeki said. "It was not just a problem for Vietnam. It was a regional problem, and a global problem."
The French Hospital outbreak was not the earliest outbreak of the new illness, but it was the first to come to the world's attention, and it was the only one that had been detected and recorded from the very first case. Starting with Chen, Vu and her colleagues had collected every scrap of clinical data that might help them understand the vicious pneumonia: throat swabs, blood samples, records of vital signs, relationships between the sick, accounts of the progression of symptoms. It was all sitting in medical charts and lab refrigerators; no one had analyzed any of it, because no one had the time.
Staring at the records, Uyeki realized that it was a potential treasure trove of critically needed information. It would need a particular kind of scientist to unlock it, though: not only an epidemiologist, but a microbiologist as well. He thought about the EIS officers he had met. Then he composed an email, asking the CDC to send Joel Montgomery.
-- -- --
The CDC that received Urbani's warnings was a different agency from the one that had scrambled to respond to anthrax seventeen months before. The attacks had shaken the CDC profoundly. It had been harshly criticized in the media and in congressional hearings for allowing the Brentwood post office to remain open, exposing thousands of workers and some of its own investigators to the spores squeezed out of the letters by the machinery and causing two of the five deaths. The criticism was partially unjust -- the decision had been made in concert with the U.S. Postal Service and without full knowledge of FBI and UAMRIID findings about the quality of the spores -- but it had stuck. It had deeply wounded the staff. And it had produced aftereffects. CDC director Jeffrey P. Koplan, who had been at the agency with one four-year break since working on smallpox in 1972, resigned at the end of March 2002. He moved to a senior position at Emory University School of Medicine, next door to the CDC. It was a logical move, and a good job; but within the national public health community, where he was widely liked, he was thought to have sacrificed his career in a bid to draw the pressure of the attacks' aftermath away from the CDC. His departure left agency veterans demoralized, imagining political interference to come.
His replacement was Julie L. Gerberding, an infectious-disease physician and HIV scientist who had joined the CDC only four years before. Gerberding had spent her career at University of California, San Francisco, where she did some of the earliest research on the threat posed to health workers by HIV. She had come to the CDC to head its Division of Healthcare Quality and Promotion, which worked on medical errors and infections occurring inside health care institutions. In early September 2002, she had agreed to take a four-month stint as acting deputy director of the National Center for Infectious Diseases, the historic heart of the CDC. The serendipity of the temporary posting put her on the short list of CDC managers -- along with Koplan, deputy director for science Dr. David Fleming, and NCID chief Dr. James M. Hughes -- who were regularly put in front of the media during the chaotic aftermath of the attacks.
To the slight surprise of the agency rank and file, she turned out to be very good at it. She was distinctive-looking, with a forelock of white hair slicing through a chin-length black bob, and on-camera she appeared focused but relaxed. She had been chief resident at UCSF and still retained the knack, essential to the position, for internalizing large amounts of data and switching with speed between different trains of thought. She seldom used notes when she spoke. When Koplan stepped down, HHS Secretary Tommy Thompson reached past
Fleming and Hughes and selected Gerberding to be successor. It was a bold choice, since she was not a CDC lifer and supporters feared the administration would frown on her career in AIDS research, but a smart one. Gerberding was forty-six and the first woman to head the CDC. Her scientific background gave her credibility among the many agency staff who had not even met her -- DHQP, the division she had headed, was a small group off to the side of the CDC's organizational chart -- and after months of their feeling targeted, Thompson's emphatic backing came as a relief.
The struggle to cope with the public alarm created by the anthrax letters -- and the thousands of biological and environmental samples, as well as hoax letters, collected during the investigation -- had revealed that U.S. public health, the bulwark against bioterrorism, was in terrible shape. Laboratories and communications networks, at the CDC and in the states, had been deprived of significant funding for years. The strain had brought the system close to breakdown, and in one case literally to failure: Early in the anthrax crisis, a major electrical line into the CDC had sizzled out from overload, halting all lab work for twelve hours.
The federal government made up for the years of underinvestment in one lump sum: In mid-2002, Congress passed a supplemental appropriation of $1.1 billion, for the CDC and the states, specifically to prepare for bioterrorism. On the CDC side, the money went to upgrade laboratories and information technology. The agency built a secure broadband network between health departments, recruited more than one hundred university, state, and private labs into cooperative agreements to provide help in emergencies, and threw hundreds of Web pages of disease information online. Private money flowed to the CDC as well. In the midst of anthrax, the agency had needed a place to coordinate the efforts of the several hundred investigators it sent into the field; lacking anything better, staff had dragged desks and bulletin boards into Auditorium A at the front of the campus and transformed it into a jury-rigged war room. The makeshift facility so appalled Bernard Marcus, an Atlanta philanthropist who co-founded the Home Depot chain, that he personally pledged to build the CDC a real emergency operations center. ("I have grandchildren. I am concerned about their health and welfare," he said when he disclosed the gift. "I can't wait for the federal government to see to that. If I can do it, I will.")
The $3.9 million result, augmented by gifts of equipment from fifteen tech manufacturers, was completed in early March. It was a softly lit, gleaming space of wood paneling, halogen drop lights, and liquidcrystal displays. Forty workstations with ergonomic chairs and flatpanel monitors faced a dais with three desks, for the logistics chief, the shift chief, and the situation commander. Behind the dais were wide plasma screens displaying news channels and GIS maps; behind the rows of workstations, on the other side of glass walls that blanked to opaque when a switch was thrown, were conference rooms wired with broadband video and audio and linked to the war rooms at HHS in Washington and the WHO in Geneva.
The contrast between the worn 1960s-era buildings above ground and the sleek basement bunker was jarring, like walking from real life into an imagined movie-set version of it. But the EOC, as it was quickly dubbed, was an oddly soothing place to work, hushed and energetic at the same time and without outside distractions.
On March 15, WHO director-general Gro Harlem Brundtland called the emerging epidemic "a worldwide health threat." She also gave it a name: SARS, for "severe acute respiratory syndrome." Following the WHO's lead, the CDC put the new EOC into crisis mode, moving full crews of staff underground to work in shifts around the clock. The war room became the nerve center of the nascent SARS emergency. The new disease called out the EIS: In short order, members of the group were dispatched to Hanoi, Toronto, Hong Kong, and Taiwan. The rest volunteered for rotating ops-center duty, to track the emerging epidemic and to monitor their colleagues abroad and make sure that they stayed well.
-- -- --
The early betting was that SARS was caused by a virus, since none of the antibiotics tried as treatments in countries had made the slightest difference to the progression of the disease. The WHO patched together a network of eleven labs around the world to look for the organism. The CDC found it. It was a coronavirus, named for a crown of spikes on the surface of the virus that could be seen through an electron microscope. Other coronaviruses were known to cause severe disease in animals and colds in humans, but this coronavirus had never been seen before.
A few days afterward Joel Montgomery and Dan Bausch, a physician with a tropical medicine degree, landed in Hanoi. The discovery of the virus -- which was still not confirmed as the cause of SARS, but was the most plausible candidate seen so far -- would give their work a target.
Vietnam's CDC equivalent was the National Institute of Hygiene and Epidemiology, or NIHE, pronounced "nee hay." NIHE was based in the old Pasteur Institute, a French colonial relic named for the premier French scientist. In another French touch, its address was 1 Yersin Street, after Alexandre Yersin, the discoverer of the plague bacillus. Unlike most of his colonial colleagues, Yersin had loved Vietnam; he had married a Vietnamese woman, settled in the country, and died and was buried there. Like the other municipal structures that had survived the French withdrawal fifty years earlier, including the Opera House and the townhouses of the gallery district, the institute's exterior was made of mellow gold stucco with delicate detail. It was a long, low building of two wings centered on a wide entrance hall with a sweeping marble staircase, and topped with a bell tower. Outwardly, it resembled a school in Provence. It looked nothing like a modern laboratory.
The inside was more modern than the outside. NIHE's specialties were virology, immunology, and disease surveillance. Its scientists were well known in Asia; it frequently hosted conferences and had its own vaccine-development arm that worked on rabies, hepatitis, and Japanese encephalitis. Still, it had never been called on to help identify a brand-new disease, and it lacked most of the high-level protections that would permit safe handling of a not-yet-understood organism. In Atlanta, the Special Pathogens Branch was performing all the SARS lab work. In Hanoi, NIHE was forced to rig a makeshift hot lab. It loaned the CDC team its influenza laboratory, an open, high-ceilinged lab with marble floors and latched wood doors pierced with small, square glass panels. It was a beautiful room, but it had no modifications that would guarantee even moderate biosafety. Joel and Dan would need to tinker with equipment and protective gear to craft a compromise that felt safe.
By email, they discussed ground rules with their Special Pathogens supervisors. The virus could cause serious disease, could be transmitted through the air, and could not currently be prevented by a vaccine. Those conclusions were obvious, and they were also troubling, because they matched three of the four conditions that Special Pathogens used to classify disease organisms as highest risk. But after looking at the scope of the worldwide epidemic -- forty-nine deaths so far among 1,323 known cases of illness -- they could not agree that the virus posed a high likelihood of life-threatening disease. That was the fourth condition. SARS did not meet it. It was a relief, and not only for their personal comfort. Concluding that SARS was high risk would have forced them to work under the highest hot-zone level of biosafety, BSL-4 -- and there was no BSL-4 lab anywhere in Vietnam. Not meeting that condition meant they could drop back to BSL-3 protections. Those were challenging enough to create: They included limiting access to the lab, making sure that building air flowed into the lab and not out of it, working inside biosafety cabinets with air circulation that flowed away from the researcher, autoclaving all the lab waste, and wearing not only basic protective gear -- gowns, gloves, and face protection -- but contained air supplies as well. Still, they were achievable. BSL-4 would have been impossible.
The researchers might have been able to get by with less. But they were working with whole blood, and it made them wary. There was as yet no evidence that SARS could be transmitted by blood, but it was impossible to ignore the lessons of two decades of AIDS, which had drilled into lab workers that blood was the most hazardous of all crude biological samples. They agreed to full protective gear, including powered air-purifying respirators with integral face shields and hoods.
"We were spinning the blood in a centrifuge that didn't have aerosol guards, so if we broke a tube, we didn't want to aerosolize the blood and breathe it in," Joel said. "And we had a safety cabinet, but the last time it had been inspected was 2001, so we didn't know if it had proper airflow."
They set up both their laptops, and in both of them started identical databases, so they could number the samples and keep track of all the information they could glean from the blood-soaked labels. They recruited two NIHE researchers to help them, since typing with bloody gloves would be too messy. And then they started opening the bags to catalogue the eight hundred tubes.
It took a week of fifteen-hour days to catalogue the tubes and centrifuge them, and divide the usable contents into three portions: one each for the Special Pathogens Branch, the WHO's lab network, and the researchers at NIHE. The work was intense but steady; the consequences of making a mistake and breaking a tube or slitting a glove were too dire to indulge their desire to rush for a result. The BSL-3 rules limited lab access to only a few people, so they were seldom bothered. It was oddly peaceful in the big, old-fashioned room, and it was easy to lose track of the outside world -- until late one weekend morning when Joel's rented cell phone buzzed.
It was news about Carlo Urbani.
-- -- --
Scott Dowell had rushed to the airport through Bangkok's twenty-four-hour traffic to meet Urbani's flight from Hanoi. By the time he arrived, it had landed. Dowell had no idea what the parasitologist looked like, but he spotted him as soon as the bus from the airplane disgorged its passengers. Urbani was taller than most of the others, but it was his expression that caught Dowell's eye: He was pale and had a grim look on his face.
Dowell and a local quarantine officer who had joined him greeted Urbani gingerly -- they were careful not to shake hands -- and then led him through an unused part of the airport to an out-of-the-way driveway. They were expecting to meet an ambulance, but there was no ambulance in sight. Its crew had stopped to get protective gear. Then they had gotten lost in the airport. It would take them ninety minutes to find the right door.
Dowell and Urbani arranged two plastic chairs about six feet apart -- close enough to hear each other over the traffic noise, but far enough, Dowell thought, to keep the risk of infection low. They talked.
"Carlo was quiet," Dowell said. "He wasn't particularly sick; he wasn't short of breath, he wasn't coughing. Mostly he had a bit of fever, and he was scared he would get a lot worse."
The ambulance, when it arrived, took them to Bamrasnadura Hospital, a state-run facility that the ministry of health had designated as the main quarantine hospital in case an ugly disease came to Thailand. It was after 2:00 a.m. They found Urbani a room that was off by itself on the third floor, away from areas where patients were being cared for. Bamras, as it is called, is a typical tropical hospital. The wards are open to the air at both ends, and there is no air-conditioning, so there was no such thing as a negative-pressure room with one-way airflow that could keep disease organisms from floating out into the hospital. Dowell and the staff hastily improvised one, propping fans in the windows to suck air in from the hallway and blow it outside.
They moved Urbani in, and checked his vital signs. He had a fever of about 100 degrees. His chest sounded clear when they listened to it. His chest X-ray was clear as well, and the level of oxygen in his blood was acceptable.
"For the most part he was not a patient who needed to be in a hospital," Dowell said. "But he was scared, and depressed. In Hanoi he had seen patients who were well in the morning and very sick in the afternoon, and he feared it would be quick."
Dowell had been working on plans for a conference in northern Thailand. It was starting in two days. He asked Mike Martin, an internist who had come to Bangkok to work on the CDC's Asian HIV program, to take over Urbani's care.
Martin was approaching forty. He had trained in Louisville, worked in Sri Lanka and Zambia, and studied in England, getting a degree from the London School of Tropical Medicine and Hygiene, before joining the EIS in 2000. He and Dowell had met during Martin's first EIS year, when they had both been sent to work on an outbreak of Ebola hemorrhagic fever in Gulu, Uganda. The five-month outbreak had sickened 428 people and killed more than half of them, including twelve Ugandan nurses and a doctor, Matthew Lukwiya, who had become Dowell's friend.
When Dowell called Martin the day after Urbani arrived, he warned him: "This could be worse than Ebola." He meant that it appeared likely to be more infectious, though the comment suggested as well how frightening the new disease could be. Martin understood. He agreed to take the case, and he went over to Bamras to meet Urbani.
"He was well," Martin said. "He had a little low-grade fever, some muscle aches and pains, perhaps some coughing. Nothing seemed bad. We had heard about mild cases of the disease, and I figured he was one of them. I thought, Maybe this is going to be OK."
Urbani, though, was still scared, and he felt isolated in the room they had stashed him in. It was at one end of the ward, at a point where the corridor ended in a cast-concrete balcony -- well away from the stairs and from other patients, but out of sight of the nurses' station or anyone else walking by. They decided to move him into the center of the floor, directly opposite the nurses. In three days, the hospital cleared the ward of patients and made the floor into an isolation suite, putting up double walls of glass that enclosed Urbani's new room and the nursing station, with a sealed one-way corridor in between. From their desk, the nurses had a clear view of Urbani in bed about eight feet away. It was a little too far, though, to see the pulse monitor and oximeter, so to read them in a hurry they kept a set of binoculars on top of the desk. To see him face-to-face required additional steps. Everyone entering the floor wore basic gear: gowns, gloves, and a fitted N-95 mask with mesh that was small enough to catch viruses before they could be inhaled. Between leaving the nursing station and entering the corridor to Urbani's room, the doctors and nurses put on an extra layer of protection: a second gown and gloves, shoe covers, and eye protection.
For more than a week, the arrangements felt like overkill. Urbani still had a low fever, and a cough that came and went. He complained of shortness of breath, and the staff put him on some supplemental oxygen, from a cannula that hung just underneath his nose. Dowell had been shipped to Taiwan, where SARS had infiltrated after being held off for weeks. He called every night to keep Urbani's spirits up. Martin went to Bamras every day.
"At the time, I thought I was going almost more for social reasons, to show him that we were paying attention and that we cared about him," he said. "Medically, he wasn't at risk."
Martin had written orders for chest X-rays to be shot every few days, to be sure Urbani's lungs were staying clear. The first few were fine. Then one, midway in the second week, was not. For the first time, he could see opaque infiltrates on the film.
Urbani's condition began to slide. Martin began listening to the daily teleconferences that linked the WHO and CDC teams working on SARS around the world, hoping for word of a treatment that might make a difference. He tried antibiotics to protect against the start of a secondary bacterial infection, newly developed antivirals, steroids because Hong Kong thought they were useful. Nothing helped. Urbani's oxygen levels were steadily declining. In the second week, they put him on a mask that forced air into his lungs.
"He would go for a day and be great, and then have a few bad days, and then a good day," Martin said. "He was strong, so strong. And mentally, he was always there."
Until, briefly, he wasn't. Pressurized oxygen is difficult to tolerate for long. The compressor noise is loud and intimate, and the whooshing air dries out the mouth and throat. For whatever reason, on a day when he had been in the hospital for more than two weeks, Urbani lifted off his oxygen mask, and his lungs collapsed.
Martin was not there. He arrived to find the Italian physician sedated and on a ventilator. The intubation had been smooth and quick, and his blood-oxygen levels were back to acceptable levels. But it was the beginning of an irreversible slide.
"He went two or three good days," Martin said. "And, you know, you're always grasping at straws. I remember thinking, in just a couple of days, he's going to turn the corner. We'll keep him comfortable, we'll do good medical care, and we'll just wait for him to come around."
He never did.
Dowell had returned to Bangkok. He and Martin were both experienced clinicians, but neither was a critical-care specialist. They had asked the WHO for extra help, and the agency had sent an Australian doctor whose specialty was intensive care. On the morning of March 29, she met with Martin to go over Urbani's condition. He had had a bad night, and she had had trouble keeping him oxygenated; she wanted Martin to know the details before she left for a few hours' break.
From the nursing station, Martin looked through the double set of windows. Urbani was lying peacefully, and there were nurses in the room with him. He picked up the phone to report to Dowell -- and out of the corner of his eye, he saw one of the nurses spring toward Urbani's bed. Martin dropped the phone and ran, out of the nursing station, through the robing room for the second set of layers, and in with Urbani. The Italian's heart had stopped. They pounced on him with defibrillator paddles, and within a minute brought him back.
A cardiac arrest is never good news, but a minute is a short amount of time to be without oxygen; brain tissue starts to die after four minutes have passed. The more troubling thing was that Martin had no idea why Urbani had coded. Without knowing the reason for the heart attack, it was difficult to predict whether it would happen again. He went back out to the nursing station, called Dowell, and began searching for Urbani's lab results from that morning, hoping to find some clue to the arrest in his blood chemistry. With his head in the chart, he heard one of the nurses bang on the window. He looked up. Urbani had coded again.
This time, getting him back took twenty minutes, an impossible length of time to be without a reliable heart rhythm. Still, Urbani rebounded: his pulse rate surged and stabilized, and his blood-oxygen began to creep back up. The team were uneasy, though, and so they stayed by his bedside. There was a moment's normalcy, and then his heart failed a third time.
Dowell had arrived at the hospital, but had no time to gown and glove. He grabbed a mask and slid into the walled nurses' station. Through the double windows, he could see Martin and a Bamras doctor and a succession of nurses, leaning stiff-armed over Urbani to give him chest compressions, backing away while one of them tried the defibrillator, waiting to see if the rhythm took hold, and then rushing in with compressions again.
The Thai doctor climbed on the bed for extra leverage. She was soaked with sweat, and her mask slipped. The sight jarred Martin out of his trance of urgency. He realized the risks the staff were running. He pulled her off the bed. She fought him. He pushed her out the door, and vaulted on the bed to take her place.
"Nobody wanted to lose Carlo," Martin said. "Nobody wanted to see him die."
After more than an hour, Martin and the nurses stepped back from the bed. There was no hint of a pulse. Urbani lay gray and unmoving. At 11:45 in the morning, they pronounced him dead.
-- -- --
Three days after Urbani died, the WHO's chief of communicable diseases announced that there had been no new cases of SARS in Vietnam for eight days. In mainland China, Hong Kong, and Canada, cases continued to climb, but it appeared the country that was the first to raise the alarm on the disease would be the first to beat it.
One day later -- it was April 2 -- an older man named Bui Duc Khiem was carried by ambulance to Bach Mai Hospital from a town named Ninh Binh, ninety-five kilometers south of Hanoi. He was tired and achy, and had a high fever, and his chest X-ray showed lung infiltrates.
The investigators went to interview him. Vietnam's SARS outbreak had been so closely associated with the French Hospital that it was unsettling to hear of a possible case coming from so far away. What they discovered was dismaying. Bui did have a connection to the French Hospital outbreak: His daughter had had an appendectomy there in March, and he had visited her. But it also seemed possible that he had started an outbreak of his own: He had been sick with the symptoms of SARS, in his hometown, for at least ten days.
For half of that time, he had been in Ninh Binh Hospital, suffering from achiness and a high fever. Doctors there had attempted to transfer him to Bach Mai, which had been designated the SARS isolation center for the entire country, but the doctors at Bach Mai had turned him away, saying he did not have all the symptoms that marked a case. Dutifully, Bui had gone home. In Ninh Binh, he was a dignitary: Before he retired, he had been a highly placed official in the local People's Committee, holding a position equivalent to deputy mayor. Hearing that he had returned from Hanoi, still ill, relatives and friends had passed by the house to bring gifts and pay their respects. After three days, feeling worse than ever, he had returned to Ninh Binh Hospital. Doctors there had taken a second chest X-ray. Spotting the distinctive signs of inflammation, they sent him back to Hanoi and insisted that he be admitted. This time, the doctors at Bach Mai agreed.
Meanwhile, at Ninh Binh Hospital, Bui's doctor -- a woman named Cuong, who was chief of internal medicine -- had developed a fever and cough of her own. Fearing she had been infected, she put herself into isolation. Her staff and her husband, who was also a doctor, had all quarantined themselves in their homes.
The doctor's case was a clear indication that a second outbreak might be starting -- and this one, unlike the French Hospital, had the potential to infect a wide community. The only people who had had contact with Johnny Chen, once he became infectious, were the doctors and nurses within one institution. But by Bui's estimate, more than a hundred people had passed through his house, and some of them had come from fifty kilometers away. The only way to find any new cases, and to keep them from spreading the disease, was to track them all down.
Joel and Dan headed south for Ninh Binh, along with Dr. Bach Huy Anh of the health ministry and Peter Horby, a British infectious disease physician who had been sent by WHO to augment Brudon's staff. The narrow road south was one lane in each direction, though "lane" was a discretionary concept to the overloaded trucks and motorbikes that leapfrogged each other down the center line and along the shoulders. It was spring, and the wet rice paddies that ran up to the road on both sides were filigreed with the incandescent green of new shoots. The villages lay back from the road, small clusters of narrow, four-story concrete houses painted sky-blue and lavender, next to walled cemeteries that held above-ground graves roofed in yellow and red. Forty kilometers out of Hanoi, the landscape changed suddenly: Narrow volcanic ridges, rough and sharp-edged, jutted out of the ground abruptly. One of them towered over the north end of Ninh Binh, topped by a Christian cross.
Ninh Binh Hospital lay in the south end of town, a two-story building that was shaped like a backwards E and fringed with fretwork balconies plastered a milky pink. The staff had prepared for the team's coming. They had washed down the rooms, using bleach as a disinfectant, and when Horby perched on the edge of a table the residue ate a hole in his trousers. The staff were also clearly unnerved to be meeting researchers from Hanoi, the center of the outbreak. They showed up wearing surgical masks -- useless against viruses, but a reliable indicator of their fear.
On the drive down, the team had decided on a two-pronged approach. They needed to find Bui's contacts, to break the chain of transmission. But to ensure there would be no additional outbreaks, they needed to coach the hospital staff in infection-control protocols: who was at risk from patients, when they needed gowns and gloves, and what sort of masks to wear. They had brought boxes of N-95s, donated by Médecins Sans fronti`eres, that had to be fitted to each wearer. They launched a training session on the spot. By the time the training session was over, half of the staff had sheepishly taken their masks off.
That night, the team negotiated a system of observation with the local communes, which were political committees that linked together households in a neighborhood. Volunteers would visit twice a day for fourteen days to make sure none of Bui's hundred visitors were feverish or coughing, and would report them if they were. The most critical contacts, though, were Bui's family. The team wanted to do those interviews themselves.
Bui lived a half-block off the road through the center of Ninh Binh, in an ochre house that had a bicycle shop on the ground floor. The next morning, the team set out to visit. The household was Bui's wife, his son-in-law -- the husband of the daughter who had been in the French Hospital -- and two teenaged nieces. The wife and the son-in-law appeared fine, though Joel took their blood and swabbed their throats to gather samples for the record. The two nieces were reluctant to meet the investigators and had to be called down from an upstairs room. Their arrival downstairs showed why: They were feverish and flushed. The team popped N-95 masks on them, and hustled them into the van to get them into isolation at the hospital; they fitted masks on the wife and son-in-law as well.
The next day, the son-in-law spiked a fever and joined the nieces in the isolation ward. Three days afterward, one of the political volunteers came to the hospital asking for the Hanoi visitors. On his daily rounds, he had found a friend of Bui's, a thirty-year-old man named Luong who lived with his parents and brother in an alley twenty yards from Bui's house. Luong drove a van for a living, and he had been in Ho Chi Minh City for several days. But he had returned the previous night, and he was not feeling well.
Luong was the first case turned up by the volunteer interrogators. The team rushed to evaluate him. He was sweating and feverish, and clearly unwell. They swabbed his throat and took his blood, fitted a mask to his face, and sent him off to Ninh Binh Hospital on the back of a motorbike.
-- -- --
Luong, who survived, was Vietnam's last recognized case of SARS. Twenty days later, after two incubation periods had passed without new cases, the WHO declared the country SARS-free. The place where the epidemic had come to light became the first to fight it off.
Other countries followed suit. China, which had fueled the epidemic by denying its origins for five months, rallied in April under great international pressure. It placed tens of thousands of people under forced quarantine and deployed roving teams of health workers empowered to stop people on the street and test them for fever. At one point, using armed forces members working around the clock, it built a 1,000-bed quarantine hospital from an empty field, in a week. Its measures were so aggressive that, though it had more than half the cases in the epidemic, it had only three times as many as Hong Kong, in a population two hundred times Hong Kong's size. The United States, which received Urbani's early warning -- and to the CDC's knowledge was never visited by a highly infectious patient such as Johnny Chen -- was equally fortunate: It had, in the end, only twenty-nine cases of SARS.
Other areas were not so lucky. Canada, where Kwan Sui Chu brought the disease February 23, battled repeated outbreaks, almost all of them in hospitals. Two Toronto hospitals were shut by Ontario's public health authority, while visitors were barred from all others -- and from nursing homes, prisons, and long-term care facilities -- unless they were relatives of sick children or critically ill adults. All hospital doors were locked and guarded, and all hospital employees were required to wear gloves, gowns, masks, and protective eyewear for the entire time they were at work.
Nevertheless, the disease continued to leak out. In mid-April, more than thirty cases were discovered among members of a Toronto charismatic religious group, the Bukas-Loob Sa Diyos community. One of its members, an eighty-two-year-old man, had been treated in the emergency department of Scarborough Grace Hospital; he sat near a seventy-six-year-old man who had shared a room with Kwan's son, Tse. Tse died March 13, and the seventy-six-year-old on March 21. The eighty-two-year-old died April 1, and when his friends and family mingled at his wake and funeral, SARS spread among them. They unknowingly passed the disease to an American man who attended a retreat with the group and fell ill after returning home to Pennsylvania. In late May, SARS flared again in Toronto, starting with a ninety-nine-year-old man who was brought to North York General Hospital north of the city with a broken pelvis. When he developed pneumonia after being hospitalized, it was not recognized as SARS. The outbreak that began with him spread to seventy-eight other patients and health care workers before being shut down. And in June, twenty women and their newborn children were quarantined after a medical student who helped deliver the babies came down with SARS two days after being released from a ten-day quarantine.
Taiwan, which appeared at first to escape the epidemic, fared worse. From late February to April, the island had only two dozen cases of the disease, all carried over the straits by business travelers from the Chinese mainland. They were all found quickly and treated, though one of them passed the infection to a nurse and three family members. And then the outbreak seemed to stop. It is possible the disease simmered without being noticed. It is probable that a false sense of confidence over vanquishing it -- combined with a lesser degree of foreign help at first, because Taiwan, in a bow to China, is not recognized by the WHO -- led to a relaxation of vigilance.
On April 16, a forty-two-year-old man who ran the laundry at Taipei's Municipal Ho Ping Hospital was admitted to a ward in his own institution with a fever and diarrhea. The man, who died April 29, lived in a room in the hospital basement and spent his free time in the emergency department, where some of his friends worked. By the time authorities realized he was a SARS case, the disease had seeded itself throughout the hospital; staff, patients, and visitors had all been exposed. More than three hundred additional cases followed, in eight other hospitals and in the community as well. Taiwan's health minister stepped down, and several hundred nurses and other health workers resigned from their jobs rather than risk treating SARS patients.
The last case in the cluster developed symptoms on June 15. It was the last case of SARS in Taiwan, and it proved to be the last in the epidemic as well. On July 5, WHO director-general Brundtland declared the fight over, for the time being.
"We do not mark the end of SARS today, but we observe a milestone: The global SARS outbreak has been contained," she said in Geneva, adding: "This is not the time to relax our vigilance. The world must remain on high alert."
Between November 2002 and July 2003, there were 8,098 cases of SARS worldwide, and 774 deaths. Twenty-one percent of the victims were health care workers.
In Vietnam, there were sixty-three cases, more than half of them doctors and nurses, and five deaths. But there were anomalies also. Though more than a third of the victims had been hospitalized at Bach Mai, SARS never spread to the staff there. Nor, after the six initial cases, did it spread in Ninh Binh, despite the prolonged face-to-face contact between Mr. Bui and his doctor and at least one hundred others. At some point, for some inexplicable reason, SARS had simply stopped.
"We can't understand why it didn't spread throughout Vietnam," Joel said. "Granted, the Vietnamese government did a remarkable job containing it, and the team did too. But I don't know who the credit should be given to, for ending the outbreak. Was it really what we did? Was there something in the population? Vietnam is an enigma."
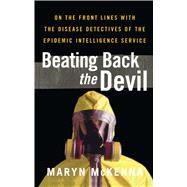
Copyright © 2004 by Maryn McKenna